The staff and volunteers at the Free Clinic in downtown Harrisonburg include (from left): Jay Landis ’54, Janice Gandy ’87, Miriam “Mim” Yoder ’08, Wes Ross ’74, Richard Stoltzfus ’59, Herbert Swartz (professor emeritus), Elaine Stoltzfus (seminar attendee), Cathy Rittenhouse ’82, Laura Rhodes ’06, Keith Gnagey ’76, and Suzy Kanode ’93. (Photo by Jon Styer)
More than 700 alumni living in the City of Harrisonburg or Rockingham County work in the healthcare field, according to EMU’s alumni database. This represents a larger concentration of alumni than in any other field of local employment.
Sentara RMH Medical Center and its affiliated offices of healthcare providers, plus a plethora of private offices offering medical, rehabilitation and wellness services, employ the vast majority of our alumni. This community-themed Crossroads did not contain sufficient space to do in-depth coverage on the vast array of our alumni in local healthcare, so we chose to focus on their work at the heart of some unique healthcare services for often-marginalized people – the kinds of services that might not be readily found in other communities.
HEALTHCARE FOR THE HOMELESS
As its name suggests, all the necessaries for Harrisonburg’s Healthcare for the Homeless Suitcase Clinic fit in a suitcase toted from place to place by the clinic’s volunteer nurse practitioner on weekly rounds of the city’s homeless shelters. At each one, the nurse practitioners offer free, on-site medical care to some of the neediest patients in a city population that ranks among the neediest in the state.
(The most recent figures from the U.S. Census Bureau put Harrisonburg’s poverty rate at 31.8%, nearly three times the statewide rate. Nearly one in five people below 64 years old in a several-county area that includes Harrisonburg lack health insurance, also according to the census bureau.)
This suitcase clinic traces its history back several years to when the director of a local homeless shelter called a meeting of health workers to talk about how to handle what they expected to be a bad flu season. Tammy Kiser ’88, assistant professor of nursing, took a few students from her community health class to that meeting. Soon thereafter, a group of those students began visiting the shelter to provide foot care to some of the men staying at the shelter, and the idea snowballed. Soon, Kiser and like-minded people at James Madison University and other local agencies began talking about how they could give more comprehensive care to the city’s homeless.
When the Healthcare for the Homeless Suitcase Clinic officially began in the summer of 2011, Kiser and others guessed they’d be seeing 50 to 80 patients per year. Instead, they saw 130. The following year, that total jumped to 245 individuals, and current year-to-date figures are on pace to remain at that level. Everything is free for the patients; the clinic’s shoestring budget has been funded by a combination of grants, church donations, private support and fundraisers. It has one paid staff member, a case manager who oversees the work of several volunteers.
“This is genuine. It’s grassroots,” says Kiser. “[The clinic] is a good fit with the whole philosophy of the EMU nursing department. It’s providing quality care to people whatever their situation is.”
But a suitcase can only fit so much, and some patients have needs beyond the clinic’s modest capabilities. When such an instance arises, staff refer them to several other providers – and hand them a bus ticket to get there – that also do their best to care for the many people in Harrisonburg who would otherwise slip through the cracks. These other agencies include the Harrisonburg Rockingham Free Clinic, the Harrisonburg Community Health Center and the local Virginia Department of Health office, all of which also have strong ties to EMU. Overviews of the work of alumni at each of these organizations follow.
“We emphasize that it’s an honor as a nurse to be able to care for people who are in vulnerable situations,” says Kate Clark ’07, an instructor in the nursing department. “That mentality makes our graduates more inclined to work with vulnerable or low-income people on a level that I don’t know a lot of other programs do.”
HARRISONBURG COMMUNITY HEALTH CENTER

Nurses Rebekah Charles ’07, “Mim” Miller Yoder ’74, and Christine Wagler ’08 are three alumni on staff at the Harrisonburg Community Health Center. (Photo by Michael Sheeler)
The Harrisonburg Community Health Center (HCHC) saw its first patient in 2008, opening as a federally qualified health center with a federal grant. A lack of providers in the area, particularly pediatricians, who accepted Medicaid was one of the major factors in its grant award. David Cockley, an adjunct professor in the nursing and MBA programs (as well as a professor in James Madison University’s health sciences program), was among the group that applied for the founding grants and remains on HCHC’s board today.
HCHC, which employed just one physician at the beginning, has seen its patient base expand rapidly. In 2011, it saw about 5,600 patients, in 2012 saw about 6,900 patients and in 2013, more than 7,400. A total of seven pediatric and adult providers – a mix of doctors, nurse practitioners and physician assistants – now work at the health center. Because a significant number of the center’s patients are non-English speakers, one full-time and two part-time Spanish interpreters work for the HCHC, and most of the center’s nursing staff are bilingual in English and Spanish. The center also employs a part-time Arabic interpreter.
Although it receives federal grants to provide healthcare to “underserved communities and vulnerable populations,” the community health center has a broader mission.
“As a federally qualified community health center, HCHC is committed to serving as a medical home for all members of our diverse community,” says HCHC director of nursing Christine Reimer Wagler ’08. “Providing comprehensive, excellent quality care, with the patient at the center of our practice, is the heart of our mission.”
The center offers sliding scale fees to patients without insurance or ability to pay for their care, and it also accepts – and welcomes – all major insurances.
In 2011, HCHC partnered with EMU to launch a Community Health Worker program. Clark, the EMU nursing instructor, was then working part-time at HCHC and helped found the program (she is also David Cockley’s daughter). Jointly administered by EMU and HCHC, the program employed four women to educate and support high-needs patients by visiting them at home. That year, HCHC also became the parent organization for the Healthcare for the Homeless Suitcase Clinic described earlier. (The homeless clinic has since spun off as its own outfit, and the grant that funded the Community Health Worker program has expired.)
The next year, HCHC opened a satellite office at the Virginia Mennonite Retirement Community that, like the main office on the east side of town, is open to the entire community.
Wagler notes that EMU’s emphasis on peace and justice also have direct tie-ins to healthcare.
“Healthcare is a justice issue,” she says. “There is no bigger issue, in my mind, than ensuring that every single person has meaningful access to quality care if they want it.
“Working in healthcare is not for the weary,” she continues. “Navigating the brokenness within the various systems can be exhausting at times. Yet amidst all of this, there is change, which creates movement. It’s an exciting time.”
Wagler finds hope in there being so many others here in Harrisonburg doing their own bit to untangle one of our society’s most difficult problems.
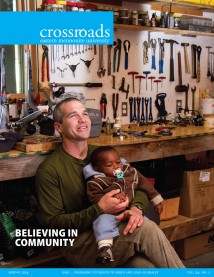
THE FREE CLINIC
Nearly 1,000 patients per year come through the doors of the Harrisonburg-Rockingham Free Clinic in downtown Harrisonburg. To qualify for services there, a person has to have an income at or below 200 percent of the federal poverty limit, be an authorized resident of Harrisonburg or Rockingham County, and have no health insurance.

Richard Stoltzfus ’59, physician at
the Free Clinic. (Photo by Jon Styer)
The clinic focuses on treatment and management of chronic health problems; nearly two-thirds of its patients have been diagnosed with three or more chronic diseases, says executive director Keith Gnagey ’76.
With just two full-time staff – Gnagey and an office manager – and 12 part-time employees, the clinic relies almost entirely on several hundred volunteers, who see patients, run lab tests, work the pharmacy and fill pretty much every other role there. The fact that volunteers perform the most skilled and fundamental roles at the Free Clinic distinguishes it from many other nonprofits.
“It’s not just putting on stamps and folding mailings. It’s about getting healthcare out the door,” says Gnagey.
Among the doctors who volunteer at the clinic are Wes Ross ’74, who sees patients there once per week and also serves as its medical director (a position that entails things like chart reviews and signing off on lab reports) and Don Martin, class of ’79, a rheumatologist who sees patients at the clinic once a month.
“There’s no way in our lifetime that all the inequities in our society are going to be resolved, but those of us who have opportunity to work on that should,” says Martin. “We can’t, as individuals, solve some of our bigger problems, but we can certainly try to address some of these things that are in our own back yard.”

Janice Gandy ‘87 (right), clinical services director at the Free Clinic. (Photo by Jon Styer)
Internist Richard Stoltzfus ’59, who used to treat coal miners in Harlan County, Ky., before he officially retired, sees patients once a week, working alongside his wife Elaine Stoltzfus, who is a health educator. (Elaine spent 1961-62 studying at EMU’s seminary.)
Clinical services director Janice Good Gandy ’87 said the rewards of working at the clinic include knowing that “you’re really helping a very needy population, and you can really see it make a difference in their lives.”
In her current role, Gandy manages the schedules of the volunteer doctors and nurse practitioners; before taking the part-time job at the clinic, she volunteered there and also taught at EMU.
The biggest challenge at the Free Clinic from a healthcare standpoint, Gandy says, is the fact that patients face so many economic and social barriers to maintaining healthy lifestyles.
“We just have to do so much education. Sometimes it’s like we do all we can, and we just hit the wall,” says Gandy, who often draws on lessons about holistic well-being, and viewing specific health problems in relation to other life circumstances, that she first learned at EMU.
Funding presents the clinic with another significant challenge. As the large majority of its budget comes in donations from people, businesses, churches and other organizations in the community, revenues took a significant hit after the 2008 recession. A “rainy-day fund” got the organization through a number of lean years, but the clinic also began to institute a modest fee structure for most patients (making the name “Free Clinic” something of a misnomer) as a way to ensure that it will remain open.

Retired English prof Jay Landis ’54 helps
process Free Clinic patients. (Photo by Jon Styer)
It is a confusing time to be in healthcare. Many people, Gnagey says, are under the impression that healthcare reform will eliminate the need for a place like the Free Clinic (“far from true,” he says, particularly given Virginia’s decision, as of press time, not to expand Medicaid eligibility). It’s not clear what, exactly, the future holds for the Free Clinic. Uncertainty about healthcare abounds; this small organization, scraping along to provide needy patients with expensive services at little to no cost, is being swept along for the ride.
“I love working for a small, local organization serving an important local need,” Gnagey adds. “It’s a privilege.” The former chair of EMU’s nursing program and provost, Beryl Brubaker, class of ’64, was a founding board member of the free clinic, serving 1991-98.
VIRGINIA DEPARTMENT OF HEALTH
Job responsibilities for Laura Quass-Ferdinand ’06, a public health nurse, include screening Medicaid patients for eligibility for in-home personal care or nursing home placement, working in the immunization and sexually transmitted infection clinics, and helping with the refugee health and baby care programs. Debbie Gullman ’73, also a public health nurse, primarily works in maternal and child health.

Kimberley Whetzel ’13, Laura Quass-Ferdinand ‘06, Debra Gullman ‘73, Kara Hulver ’07, Wanda Revercomb ’86, Stephanie Kanagy ’10 and Fonda Cassidy ’86. (Photo by Jon Styer)
While the health department performs a wide variety of functions – it also enforces health code in restaurants and has an entire environmental health arm – public health nurses like Gullman and Quass-Ferdinand mainly provide preventive healthcare to populations that otherwise would have none. (Undocumented immigrants, many of whom lack insurance and who are ineligible for Medicaid, for example, comprise much of the obstetrical practice.)
“I like that I can be involved with people who are at the margins,” says Gullman, adding that public health nursing is “really nursing and social work [mixed] together.” The EMU nursing program’s strong focus on the social dynamics of health and wellness translate well to this kind of nursing, adds Quass-Ferdinand.
— Andrew Jenner ’04